November 2, 2010, researchers from the Veterans Affairs Medical Center at the University of California, San Francisco, published a study in the Annals of Internal Medicine titled (1):
The Epidemiology of Pain During the Last 2 Years of Life
The study included 4,703 older adults with mean age of 75.7 years at the time of their deaths. These subjects were evaluated for the presence of clinically significant pain, as indicated by a report that the participant was “often troubled” by pain of at least moderate severity. Their records showed that the prevalence of such pain 24 months before death was 26%. The pain prevalence remained flat until 4 months before death, then the pain increased, reaching 46% in the last month of life.
Importantly, the prevalence of pain in the last month of life was 60% among patients with arthritis versus 26% among patients without arthritis and did not differ by terminal diagnosis category (cancer, heart disease, frailty, sudden death, or other causes).
The authors concluded:
“Although the prevalence of pain increases in the last 4 months of life, pain is present in more than one quarter of elderly persons during the last 2 years of life.”
“Arthritis is strongly associated with pain at the end of life.”
This study indicates that a non-fatal condition, arthritis, significantly affects the quality of life in the elderly.
•••••
A number of well-respected reference texts indicate that the incidence of osteoarthritis is strongly associated with single event macro-trauma, repeated micro-trauma, alignment problems, and age. Such texts include:
- The Human Spine in Health and Disease, by Georg Schmorl and Herbert Junghanns (2).
- The Cervical Syndrome by Ruth Jackson (3).
- Anatomico-Roentgenographic Studies of the Spine by Lee Hadley (4).
- Managing Low Back Pain by Harry Kirkaldy-Willis (5).
- Clinical Implications of Normal Biomechanical Stresses on Spinal Function by Herbert Junghanns (6).
A 1993 study published in the journal Injury (7) showed strong evidence that a single motor vehicle collision accelerates the process of disc degenerative disease of the cervical spine.
A 1997 study published in the Journal of Orthopedic Medicine (8) showed that a single motor vehicle collision accelerated degenerative changes in the cervical spine by about 10 years earlier compared to the control group.
A 2004 study published in the European Spine Journal (9) showed that the repetitive heading of soccer balls accelerates degenerative changes in the cervical spine by 10–20 years earlier than that of the normal population.
A 2009 study published in the Journal of Physical Activity and Health (10) showed that knee and hip arthritis is over 3 times more prevalent in retired NFL players than in the general U.S. population of the same age.
PATHOPHYSIOLOGY
An excellent discussion of the pathophysiological process leading to spinal osteoarthritis is presented by the late (d. 2006) William H Kirkaldy-Willis, MD. Dr. Kirkaldy-Willis was Emeritus Professor, Department of Orthopaedic Surgery, University Hospital, University of Saskatchewan College of Medicine. In his 1988 (second edition) book Managing Low Back Pain, there are 19 international multidisciplinary distinguished contributing authors (5). Dr. Kirkaldy-Willis authored a chapter in the book titled:
“The Three Phases of the Spectrum of Degenerative Disease”
Dr. Kirkaldy-Willis describes how spinal segments are comprised of a three-joint complex: the two posterior facet joints and the intervertebral disc. He notes that the three joints always work together. Consequently, injury or stress to any single component of the three-joint complex will mechanically affect the other two components. His breakdown of the three phases of spinal degenerative disease is as follows:
First Phase of Spondylosis
“Dysfunction”
In the first phase, the normal function of the three-joint complex is interrupted as a consequence of injury or chronic stress. This causes the posterior musculature of the involved segment to go into a state of hypertonic contraction. This restricts normal movement. The hypertonic contraction of the muscles also causes muscle ischemia, causing pain. The muscle hypertonicity also causes a slight misalignment of the posterior facet joints, which is known as a “subluxation.” Eventually tissue fibrosis begins to appear.
Second Phase of Spondylosis
“Instability”
If the first phase is allowed to persist, the second phase will eventually ensue. In the second phase, there is abnormal increased movement. Laxity of the posterior joint capsule and of the annulus fibrosus is seen in anatomical sections. Local fibrosis is problematic because “the collagen of scar tissue is not as strong as normal collagen.” Therefore, there is an increased propensity for additional injury, inflammation, pain, and muscle hypertonicity.
Third Phase of Spondylosis
“Stabilization”
If the second phase is allowed to persist, the third phase will eventually ensue. In the third phase, degenerative changes begin to appear. As the degenerative changes advance, the unstable segment regains its stability because of fibrosis and osteophytes form around the posterior joints and within and around the disc. In this stabilization phase, the facet joints will progress through the following sequence:
Synovitis
↓
Degeneration of Articular Hyaline Cartilage
↓
Development of Intra-articular Adhesions
↓
Increasing Capsular Laxity
↓
Subluxation of the Joint Surfaces
↓
Formation of Subperiosteal Osteophytes
↓
Enlargement of Both Inferior and Superior Facets
↓
Ultimately Greatly Reduced Movement
Simultaneous with this sequence of changes in the facet joints, there are parallel changes in the intervertebral disc. These changes follow this sequence:
The Development of Small Circumferential Tears in the Annulus Fibrosis
↓
The Circumferential Tears in the Annulus Become Larger and Coalesce to form Radial Tears that Pass From the Annulus to the Nucleus Pulposus
↓
Eventual Internal Disruption of the Disc
↓
Disc Degeneration with Disc Resorption
↓
Peripheral Osteophytes Around the Circumference of the Disc
↓
Ultimately Greatly Reduced Movement
Dr. Kirkaldy-Willis notes that the “greatly reduced motion” associated with spinal degenerative disease opens Melzack’s and Wall’s “pain gate,” accounting for the increased pain that is often associated with osteoarthritis (12).
•••••
A more recent comprehensive review of osteoarthritis appeared in the American Journal of Physical Medicine and Rehabilitation in 2006, titled (11):
Osteoarthritis
Epidemiology, Risk Factors, and Pathophysiology
The authors, Susan V Garstand, MD and Todd P Stitik, MD, are from the University of Medicine and Dentistry of New Jersey. In this article, Drs. Garstand and Stitik note that osteoarthritis is “the clinical and pathologic outcome of a range of disorders that results in structural and functional failure of synovial joints. Osteoarthritis occurs when the dynamic equilibrium between the breakdown and repair of joint tissues is overwhelmed.”
Drs. Garstand and Stitik note that osteoarthritis is the most prevalent form of arthritis and a major cause of disability in people aged 65 and older. Osteoarthritis affects the majority of adults over age 55.
Garstand and Stitik note that the incidence of osteoarthritis is influenced by both systemic and local factors:
Systemic Factors:
• Ethnicity
• Age: “The presence of radiographic osteoarthritis rises with age at all joint sites.”
• Gender
• Hormonal Status
• Genetic Factors; osteoarthritis has a major genetic component
• Bone Density
• Nutritional Factors:
There is evidence that osteoarthritis is linked to free radicals, and that high dietary antioxidants (especially vitamins C and D) are protective against the development of osteoarthritis. “Chondrocyte senescence is thought to be the result of chronic oxidative stress.”
Local Factors: Local factors “result in abnormal biomechanical loading of affected joints.”
• Obesity
• “Altered joint biomechanics”
• ligamentous laxity
• malalignment
• impaired proprioception. With aging, there is a decline in proprioception, causing decreased neurologic responses, impairing proprioceptive joint-protective mechanisms. Consequently, reduced proprioception advances osteoarthritis.
• muscle weakness
• Prior joint injuries
• Occupational Factors
• Effects of sports and physical activities
• Developmental abnormalities
Garstand and Stitik note that if systemic factors are present, the joints are vulnerable, and thus local biomechanical factors will have more of an impact on joint degeneration and osteoarthritis.
•••••
Essential Fatty Acid Connection
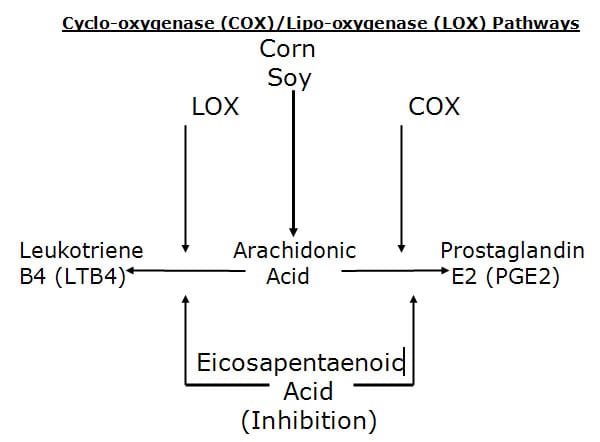
In his 2008 book Toxic Fat, biochemist Barry Sears (13) describes how the omega-6 fatty acid arachidonic acid is biochemically converted into the pro-inflammatory eicosanoid hormone prostaglandin E2 (PGE2).
Cyclo-oxygenase (COX)/Lipo-oxygenase (LOX) Pathways
The conversion of the omega-6 fatty acid arachidonic acid is biochemically converted into the pro-inflammatory eicosanoid hormone prostaglandin E2 (PGE2) and is important in a discussion of osteoarthritis because a number of studies have implicated prostaglandin E2 in the accelerated degradation of cartilage. For example, in 2002 the journal Neurosurgery Focus published a study linking disc degeneration to prostaglandin E2 (14). Later in 2002, the journal Spine published a study linking intervertebral disc herniation to the enzyme cyclo-oxygenase-2, which converts the toxic fat arachidonic acid to prostaglandin E2 (15).
Also in 2002, the journal Arthritis & Rheumatism (16) published a study showing that the pathologic indicators manifested in human osteoarthritic cartilage could be significantly abrogated by exposure of the cartilage to omega-3 fatty acids. This is important because omega-3 fatty acids, especially the omega-3 eicosapentaenoic acid (EPA), is known to inhibit the conversion of arachidonic acid into prostaglandin E2. Neither omega-6 nor omega-9 (such as olive oil) could stop the cartilage breakdown biomarkers. These authors concluded that omega-3 fatty acids play a role in halting or slowing degradative and inflammatory factors that contribute to the progression of osteoarthritis. Specifically, they state:
“Dietary supplementation with n-3 PUFA may prove useful in both quiescent and active arthritis.”
“Our findings support the results of epidemiologic and clinical studies that have demonstrated dietary supplementation with omega-3 fatty acids to be beneficial in reducing pain and inflammation in human arthritic diseases.”
“It has long been recognized that dietary supplementation with fish oils that are enriched with n-3 PUFAs can provide benefit in the treatment of arthritis.”
•••••
Nutritional Management
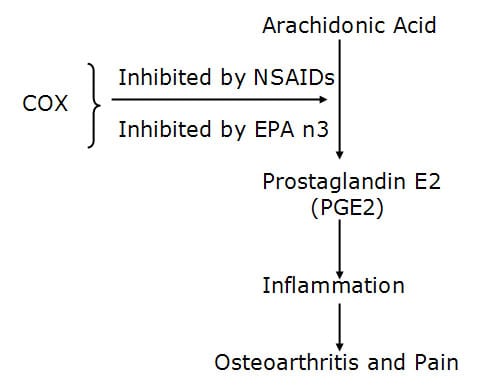
In 2006, Leslie Cleland and colleagues published a study pertaining to the utilization of omega-3 fish oil prescription for the purposes of achieving an anti-inflammatory state in arthritis sufferers (17). The pain of arthritis is primarily caused by prostaglandin E2 (PGE2), which is derived from the omega-6 fatty acid arachidonic acid through the activity of the enzyme COX. Nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit the COX enzyme. Dr. Cleland restates that the omega-3 fatty acid found in fish oil, eicosapentaenoic acid (EPA), not only inhibits the conversion of arachidonic acid to the pro-inflammatory eicosanoid prostaglandin E2 (PGE2), but also inhibits the conversion of arachidonic acid into another pro-inflammatory eicosanoid, leukotriene B4 (LTB4). Cleland and colleagues suggest that as a therapeutic agent, EPA should be superior to NSAIDs because NSAIDs do not inhibit the lipoxygenase (LOX) pathway.
Cleland and colleagues state that in order to achieve an anti-inflammatory state for arthritis patients, they would need to consume a minimum of 2,700 mg of long chain omega-three fatty acids per day, and they would have to do so daily for a minimum of 2-3 months.
Also in 2006, Dr. Joseph Maroon, the neurosurgeon for the Pittsburgh Steelers, published a study in the journal Surgical Neurology titled (18):
Omega-3 Fatty acids (fish oil) as an anti-inflammatory:
An alternative to nonsteroidal anti-inflammatory drugs for discogenic pain
This paper won first prize in the poster competition at the American Association of Neurological Surgeons Annual Meeting, New Orleans, LA, April 2005. Dr. Maroon is a specialist in the management of degenerative spinal disease in the Department of Neurological Surgery at the University of Pittsburgh Medical Center.
In this study, Dr. Maroon notes that NSAIDs are the most common cause of drug-related morbidity and mortality reported to the FDA and other regulatory agencies around the world. The use of NSAIDs is associated with extreme complications, including gastric ulcers, bleeding, myocardial infarction, stroke, and even death. “More than 70 million NSAID prescriptions are written each year, and 30 billion over-the-counter NSAID tablets are sold annually.” “The agent best documented by hundreds of references in the literature for its anti-inflammatory effects is omega-3 EFAs found in fish and in pharmaceutical-grade fish oil supplements.”
In this study, after 75 days on fish oil, 59% of patients who were taking NSAIDs for chronic spinal pain and who had spinal osteoarthritis, were able to discontinue their prescription NSAIDs, and 88% stated they were satisfied with their improvement and that they would continue to take the fish oil. Dr. Maroon concluded:
“Omega-3 essential fatty acid fish oil supplements appear to be a safer alternative to NSAIDs for treatment of nonsurgical neck or back pain.”
Mechanical Management
Drs. Garstand and Stitik (11) indicate that there exists biomechanical factors in the development of osteoarthritis, including altered joint biomechanics, reduced motion, ligamentous laxity, malalignment, impaired proprioception, and muscle weakness. Chiropractic training and clinical practice emphasizes and specializes in the diagnosis and management of these problems.
Additionally, Dr. Kirkaldy-Willis (5) indicates that it is during the First Phase or Dysfunction Phase of spinal degeneration when most patients experience their first episode of back pain. Importantly, Dr. Kirkaldy-Willis indicates that the pathological changes during the First Phase are minor and potentially reversible. Dr. Kirkaldy-Willis suggests that spinal manipulation is a viable approach for the management of this first phase of spinal degeneration, noting:
“Manipulation is an art that requires much practice to acquire the necessary skill and competence. Few medical practitioners have the time or inclination to master it. This modality has much to offer to the patient with low back pain, especially in the earlier stages during the phase of dysfunction. The majority of patients are first seen while in this phase. Most practitioners of medicine, whether family physicians, or surgeons, will wish to refer their patients to a practitioner of manipulative therapy with whom they can cooperate, whose work they know, and whom they can trust. The physician who makes use of this resource will have many contented patients and save himself many headaches.”
Although this quote suggests that joint manipulation is most beneficial during the earliest phases of joint degeneration, a number of studies document that joint manipulation is excellent or even superior in the management of patients suffering from chronic back pain (19, 20, 21). Long-term chronicity of spinal pain (up to 8.3 years, (21)), suggests that these patients are not in earlier phases of spinal degeneration, but are probably more in the phase of stabilization with osteoarthritic changes.
Summary
The eicosanoid hormone prostaglandin E2 is best known as a pain mediator, but it is also linked to the development of osteoarthritis. Studies indicate that an effective management for both the pain and the development of osteoarthritis is supplemental omega-3 fatty acid fish oil. Chiropractors are well trained in the biochemistry and application of such omega-3 supplements.
Biomechanically, spinal osteoarthritis begins as an injury or stress that causes local muscular hypertonicity, segmental joint dysfunction and misalignment. This early stage of pathophysiology is ideally aborted with spinal manipulation. Later stages of the osteoarthritic pathophysiological response, involving altered proprioception, muscle weakness, and reduced mobility from stabilization are also improved with joint manipulation, exercise, and targeted tissue work. The modern chiropractor is well trained in each of these clinical approaches.
Additionally, today’s modern chiropractor has management skills in several of the systemic factors in osteoarthritis, including obesity, free radical damage, repetitive strains, and ergonomics.
REFERENCES
1) Smith AK, Cenzer IS, Knight SJ, Puntillo KA, Widera E, Williams BA, Boscardin WJ, Covinsky KE; Annals of Internal Medicine; The epidemiology of pain during the last 2 years of life; November 2, 2010;153(9):563-9.
2) Schmoral G, Junghanns H; Schmorl’s and Junghanns’ The Human Spine in Health and Disease; Grune & Stratton; 1971.
3) Jackson R, The Cervical Syndrome, Thomas, 1978.
4) Hadley LA, Anatomico-Roentgenographic Studies of the Spine, fourth printing, Charles Thomas, 1979.
5) Kirkaldy-Willis H; Managing Low Back Pain, Second Edition, Churchill Livingstone, 1988.
6) Junghanns H; Clinical Implications of Normal Biomechanical Stresses on Spinal Function; Aspen, 1990.
7) Hamer AJ, Gargan MF, Bannister GC, Nelson RJ. Whiplash injury and surgically treated cervical disc disease. Injury. 1993 Sep;24(8):549-50.
8) Gargan MF, Bannister GC. The Comparative Effects of Whiplash Injuries. The Journal of Orthopaedic Medicine, 19(1), 1997, pp. 15-17.
9) Kartal A, Yldran B, Enköylü A, Korkusuz F; Soccer causes degenerative changes in the cervical spine; European Spine Journal, February 2004, 13(1):76-82.
10) Golightly YM, Marshall SW, Callahan LF, Guskiewicz K; Early-Onset Arthritis in Retired National Football League Players; Journal of Physical Activity and Health, 2009, 6, 638-643.
11) Garstand SV, Stitik, TP; Osteoarthritis: Epidemiology, Risk Factors, and Pathophysiology; American Journal of Physical Medicine and Rehabilitation; November 2006, Vol. 85, No. 11, pp. S2-S11.
12) Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965 Nov 19;150(699):971-9.
13) Sears B; Toxic Fat; 2008.
14) Martin MD, Boxell CM, Malone DG; Pathophysiology of lumbar disc degeneration: A review of the literature; Neurosurgery Focus; Vol. 13, No. 2, August 2002.
15) Miyamoto H, Saura R, Doita M, Kurosaka M, Mizuno K; Role of Cyclo-oxygenase-2 in Lumbar Disc Herniation; Spine; Vol. 27, No. 22, November 15, 2002, pp. 2477-2483.
16) Curtis CL, Rees SG, Little CB, Flannery CR, Hughes CE, Wilson C, Dent CM, Otterness IG, Harwood JL, Caterson B; Pathologic indicators of degradation and inflammation in human osteoarthritic cartilage are abrogated by exposure to n-3 fatty acids; Arthritis & Rheumatism; Volume 46, Issue 6, 2002, pp 1544-1553.
17) Cleland LG, James MJ, Proudman SM; Fish oil: what the prescriber needs to know; Arthritis Research & Therapy; Volume 8, Issue 1, 2006.
18) Maroon JC, Bost JW; Omega-3 Fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain; Surgical Neurology; 65 (April 2006) 326– 331.
19) Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low back Pain; Canadian Family Physician; March 1985, Vol. 31, pp. 535-540.
20) Meade TW, Dyer S, Browne W, Townsend J, Frank AO; Low back pain of mechanical origin: Randomized comparison of chiropractic and hospital outpatient treatment; British Medical Journal; Volume 300, JUNE 2, 1990, pp. 1431-7.
21) Giles LGF, Muller R; Chronic Spinal Pain: A Randomized Clinical Trial Comparing Medication, Acupuncture, and Spinal Manipulation; Spine, July 15, 2003; 28(14):1490-1502.