Back Pain, Acute Soft Tissue Injuries, Mobilization, & Fibromyalgia A Review Of The Literature
Medicine and Science in Sports and Exercise. Oct. 1986;18(5):489-500.
John Kellett
FROM ABSTRACT:
The pathological processes [of soft tissue injury and repair] at a cellular level are described in three phases: acute inflammatory, repair, and remodelling.
The management of acute soft tissue trauma is embodied in the acronym RICE for rest, ice, compression, and elevation during the first 48 to 72 h.
Additional benefit from anti-prostaglandin medications has not been clearly demonstrated in clinical trials, and if used, these medications should be restricted to the first 3 days.
Cryotherapy (crushed ice) for 10 to 20 min, 2 to 4 times/day for the first 2 to 3 days is helpful in promoting early return to full activity.
Early mobilization, guided by the pain response, promotes a more rapid return to full activity.
Early mobilization, guided by the pain response, promotes a more rapid return to full functional recovery.
Progressive resistance exercises (isotonic, isokinetic, and isometric) are essential to restore full muscle and joint function.
Rehabilitation is complete when the injured and adjacent tissues are restored to full pain-free functional capacity under competitive conditions in association with the necessary level of cardiovascular respiratory fitness.
THIS AUTHOR ALSO NOTES:
A common classification of soft tissue injuries is based on severity:
1) Grade 1 (first degree)
"Mild pain at the time of injury or within 24 h of injury, especially when stress is applies to the injury; local tenderness may or may not be present."
2) Grade 2 (second degree)
"The person notices pain during activity and usually has to stop; pain and local tenderness are moderate to severe when the injury is stressed."
3) Grade 3 (third degree)
"Complete or near complete rupture or avulsion of at least a portion of a ligament or tendon with severe pain or loss of function; a palpable defect may be present; stressing a ruptured ligament may, paradoxically, be painless due to the loss of continuity of the tissue."
In a third degree ligament sprain, "the ligament may appear intact macroscopically yet have complete loss of load-carrying ability."
Third degree ligament injury may require surgical management.
In inter-muscular hematoma, the blood tracks distally from the site of injury and appears as a bruise some distance from the site of injury, after some time.
Intra-muscular hematoma remains confined by epimysium and may take three times longer to heal than inter-muscular hematoma.
In ligaments, microscopic collagen fiber failure begins at 7 to 8% strain.
Ligament strain greater than 7 to 8% results in failure of the ligament to resume its original length after removal of the load (plastic deformation), and to more extensive collagen failure.
Ligaments strains as high as 20 to 40% can occur before signs of failure are apparent.
"Continuity of ligaments may be macroscopically apparent (e.g. arthroscopically) even with complete loss of the load-carrying capacity of the ligament."
"The micropathology of acute soft tissue trauma has been investigated. Healing of ligaments and soft tissue injuries in general has been shown to occur by fibrous repair (scar tissue) and not by regeneration of the damaged tissue."
[The Fibrosis Of Repair]
The phases of soft tissue injury repair are:
Phase 1:
The Acute Inflammatory or Reaction Phase.
Lasts up to 72 hours.
Characterized by vasodilation, immune system activation of phagocytosis to remove debris, the release of prostaglandins and inflammation.
Prostaglandins play a prominent part in pain production and increased capillary permeability (swelling).
The wound is hypoxic, but macrophages can perform the phagocytosis duties anaerobically.
Phase 2:
The Repair or Regeneration Phase.
48 hours to 6 weeks.
Characterized by the synthesis and deposition of collagen.
The collagen that is deposited is "not fully oriented in the direction of tensile strength.
Collagen fibers tend to contract between 3 and 14 weeks after injury, and perhaps for as long as 6 months, decreasing tissue elasticity. [This is probably why we note reduced range of motion during this phase.]
This phase is "largely one of increasing the quantity of the collagen" but this collagen is not laid down in the direction of stress.
Phase 3:
The Remodeling Phase.
This phase may last up to "12 months or more."
"The collagen is remodeled to increase the functional capabilities of the tendon or ligament to withstand the stresses imposed upon it."
"It appears that the tensile strength of the collagen is quite specific to the forces imposed on it during the remodeling phase: i.e. the maximum strength will be in the direction of the forces imposed on the ligament." [This could argue for the need for specific line-of-drive joint adjustments.] This phase is largely "an improvement of the quality" (orientation and tensile strength) of the collagen.
"Normal ligaments are composed of type I collagen, whereas damaged (and healed) ligaments contain a large proportion of immature type III collagen which is deficient in the number of cross-linkages between and within the tropocollagen subunits."
The remodeled scar is deficient in both content and quality 40 weeks after injury, as there is a plateau in scar collagen concentration at about 70% of normal.
Acute inflammation is beneficial when one has acute infection. However, the "acute inflammatory phase of the body's response to trauma is apparently of no benefit." [Most Important]
"Numerous studies have shown the effectiveness of ice therapy in reducing the pain and period of disability to soft tissue injuries."(4 references)[Important]
In contrast, "early heat treatment leads to an increase in the blood flow to the injured area with an exaggerated acute inflammatory response." [Important]
"The advantages of cryotherapy in treating soft tissue injuries have been well documented." Ice within 48 hours of injury reduces disability of ankle sprains from 15 days to 10 days.
Cryotherapy is superior to heat, especially when applied within 24 hours of injury.
Cryotherapy should be limited to a maximum duration of 30 minutes.
"The use of anti-prostaglandin medications or nonsteroidal anti-inflammatory drugs (NSAIDs) in the management of acute soft tissue injury has become increasingly common in recent years despite a lack of adequate clinical studies to support such a practice." [Important]
Prostaglandins, especially E2, are responsible for the acute inflammatory response to trauma. [Very Important]
The use of anti-prostaglandin medications or nonsteroidal anti-inflammatory drugs (NSAIDs) should be used for no more than 72 hours or they become detrimental to the second phase of healing. [Important]
"It is well to remember that all of these types of medications have adverse effects, some minor (e.g. gastrointestinal intolerance) and some major (e.g. fatalities from bone marrow suppression)." [This is really important: common pain drugs suppress the bone marrow, the sole producer of immune system cells. In another context, taking these pain drugs when suffering from colds or flu would suppress the immune system's ability to neutralize the pathogens.] The use of these drugs "should be restricted to a maximum of 3 days following injury."
Corticosteroids have been shown to cause destructive changes in articular cartilage. "Steroids have a deleterious effect on collagen and direct injection into collagen may produce a permanent decrease in tensile strength." The use of steroids for soft tissue injury has "no sound biological basis." Steroids delay collagen repair. Steroids "retard fibroblastic activity and may well delay healing." "Corticosteroids have little part to play in the management of soft tissue injuries."
BENEFITS OF EARLY MOBILIZATION
1) Improvement of bone and ligament strength, reducing recurrence of injury.
2) The strength of repaired ligaments is proportional to the mobility of the ligament, resulting in larger diameter collagen fiber bundles and more total collagen.
3) "Collagen fiber growth and realignment can be stimulated by early tensile loading of muscle, tendon, and ligament." [Important]
4) Collagen formation is not confined to the healing ligaments, but adheres to surrounding tissues. The formation of these adhesions between repairing tissues and adjacent structures is minimized by early movement.
5) With motion, "joint proprioception is maintained or develops earlier after injury, and this may be of importance in preventing recurrences of injuries and in hastening full recovery to competitive fitness." [Important, especially for chiropractors]
6) The nutrition to the cartilage is better maintained with early mobilization.
ADVERSENESS OF IMMOBILIZATION
1) A decrease in aerobic capacity.
2) Muscle wasting and loss of strength.
3) One study showed that 8 weeks of immobilization of the anterior cruciate ligament delayed the return to full tensile strength for more than one year.
4) "Immobilization leads to a higher incidence of avulsion fractures of bony attachments of ligaments rather than ligament failure." [Important]
MANAGEMENT RECOMMENDATIONS:
1) "The principles of management of acute soft tissue injuries have been embodied in the acronym RICE (for rest, ice, compression, and elevation) during the first 48 to 72 hours following injury."
2) Following this acute inflammatory phase and largely guided by the pain response of the patient, early mobilization is commenced, based upon the premise that the stress of movement on repairing collagen is largely responsible for the orientation and tensile strength of the tendons and ligaments.
3) The goal of stressing repairing tissues with controlled motion is to induce adaptive response of functionally stronger connective tissues. However, excessive stressing of the repairing tissues may result in further damage. Consequently, any sign or symptom which suggests a worsening of the injury (severe pain) is a clear indication to reduce the motion stress on the tissues.
4) "The masking of such symptoms by analgesics is contraindicated." [Important]
5) Drinking alcohol increases local hemorrhage and the acute inflammatory response, and should therefore be avoided.
KEY POINTS FROM DAN MURPHY
1) Ligaments collagen fibers begin to fail at 7 to 8% strain.
2) Ligament strains as high as 20 to 40% can occur before signs of failure are apparent.
3) The healing of ligaments and soft tissue injuries in general has been shown to occur by fibrous repair or scar tissue, [The Fibrosis Of Repair] and not by regeneration of the damaged tissue.
4) There are three primary phases of soft tissue injury repair:
A) Phase 1, The Acute Inflammatory or Reaction Phase.
Lasts up to 72 hours, is characterized by pain and swelling, and mediated primarily by prostaglandin E2.
B) Phase 2, The Repair or Regeneration Phase.
48 hours to 6 weeks, characterized by the synthesis and deposition of collagen, but this collagen is not fully oriented in the direction of tensile strength.
C) Phase 3, The Remodeling Phase.
This phase may last up to "12 months or more."
"The collagen is remodeled to increase the functional capabilities to withstand the stresses imposed upon it;" this remodeling occurs in response to specific forces applied to the tissues.
5) Healed ligaments still have problems. There are residual weaknesses as compared to normal ligaments because of reduced cross-linkages and a plateau in scar collagen concentration at about 70% of normal.
6) When one has an infection, acute inflammation is beneficial because it helps the body neutralize the pathogen. However, the "acute inflammatory phase of the body's response to trauma is apparently of no benefit," and results in adverse fibrosis. Early management should therefore include ice, not heat.
7) The use of anti-prostaglandin medications or nonsteroidal anti-inflammatory drugs (NSAIDs) in the management of acute soft tissue injury should NOT be used for more than 72 hours or they become detrimental to the second phase of healing. [Important]
8) Common pain drugs suppress the bone marrow [production of immune system cells]. [This is really important]
9) Corticosteroids damage articular cartilage, weaken the collagen repair, delay collagen repair, produce a permanent decrease in collagen strength, and should therefore never be used in the management of soft tissue injuries.
10) Early mobilization of soft tissue injuries improves the healing of bone, cartilage, tendon, ligament; reduces the adverseness of adhesions, and restores joint proprioception.
11) Immobilization of soft tissue injures decreases aerobic capacity, causes muscle wasting and loss of strength that may delay full recovery for a year or more.
Chiropractic Adjuncts To Managing Patients With Fibromyalgia Syndrome
Fibromyalgia Syndrome is the third most commonly diagnosed rheumatologic disorder, following osteoarthritis and rheumatoid arthritis. Fibromyalgia is characterized by widespread pain and tenderness, fatigue, morning stiffness, and sleep disturbance. Fibromyalgia is often disabling. Fibromyalgia is often treatment resistant. Fibromyalgia can be triggered by trauma (Greenfield, Waylonis, Buskila, Neumann). Studies report that between 25% and 50% of subjects with fibromyalgia recall physical trauma immediately prior the onset of their symptoms (Al-Allaf).
Chiropractors usually manage patients with fibromyalgia by attempting to enhance the quality of mechanical neurological afferentation by improving the sagittal and horizontal planes of spinal posture and motion. However, these efforts will often worsen patient symptoms, at least temporarily.
This article reviews several adjunct approaches to the management of patients with fibromyalgia syndrome.
MALIC ACID and MAGNESIUM
In 1992, Abraham and Flechas propose that fibromyalgia is caused by a deficiency of substances needed for ATP synthesis. The nociceptive nervous system requires a steady flow of ATP to remain subthreshold. Therefore, reductions in ATP supplies could account for the lowered pain thresholds that fibromyalgia patients experience.
Abraham and Flechas explain the synergistic role of magnesium and malic acid in the genesis of ATP. They detail the biochemistry of how reductions in magnesium and malic acid would result in APT deficiency.
Abraham and Flechas then treat 15 fibromyalgia patients with daily 300-600 mg of magnesium plus 1200-2400 mg malic acid. "All patients reported significant subjective improvement of pain within 48 hours of starting" supplementation.
In 1995, Russell et al in a randomized, double blind, placebo controlled, crossover study, also used magnesium and malic acid to treat 29 patients with fibromyalgia, noting "significant reductions in the severity of all 3 primary pain/tenderness measures were observed." Better results were observed in those taking 600 mg of magnesium and 2400 mg of malic acid, as compared to those who took lower doses. The authors note that this supplementation should continue for al least 2 months, and often for as long as 6 months.
THE SEROTONIN PATHWAY
In 2004, Borut Banic and colleagues, writing in the journal Neurology, present extensive evidence suggesting that fibromyalgia is the consequence of reduced levels of the brain neurotransmitter serotonin.
In 1998, osteopath John H Juhl also proposed that fibromyalgia could be related to reduced serotonin. He notes that researchers have found low serum levels of serotonin in fibromyalgia patients. Low serum serotonin levels have been found to have an inverse correlation with clinical measures of pain.
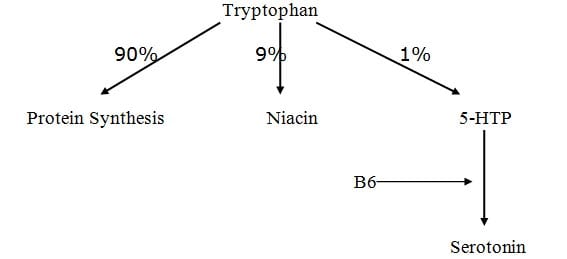
The serotonin pathway begins with the essential amino acid tryptophan.
Tryptophan is the least common of the 8 essential amino acids, accounting for about 1% of protein content.
After absorption, about 90% of tryptophan is used at the peripheral tissues for protein synthesis.
About 9% of absorbed tryptophan is used to produce niacin. The RDA for niacin is 15 mg. It takes 60 mg of tryptophan to produce 1 mg of niacin. This is important, because if niacin levels are adequate in the diet, the body will not need to use this 9% to make niacin.
In fact, the higher the dietary levels of niacin, the less tryptophan is converted to this pathway. This increases the tryptophan available to be converted to serotonin.
About 1% of absorbed tryptophan is converted to serotonin.
In the body, tryptophan is converted to 5-hydroxy-tryptophan (5-HPT). 5-HTP easily crosses the blood-brain barrier for conversion to serotonin in the central nervous system. The conversion of 5-HPT to serotonin requires vitamin B6. Consequently, inadequate levels of B6 impair the conversion of tryptophan to serotonin.
Currently, tryptophan is available by prescription only in the United States. However, 5-HTP is sold, and as noted above, still crosses the blood brain barrier for conversion to serotonin. Commercially, 5-HTP is extracted from the seeds of Grifonia simplicifolia, a plant grown in West Africa.
Dr. Juhl notes 2 published studies where supplementation of 5-HTP in the dose of 100 mg 3 times per day in patients with fibromyalgia resulted in significant improvement of clinical symptoms after 30-90 days. The effective daily dose range appears to be 200-1000 mg total per day, and that it should be taken with meals.
These patients should also be given vitamin B6 to increase conversion of 5-HTP to serotonin, and niacinamide to inhibit the need for tryptophan to convert to niacin.
Dr. Rodger Murphree supports the tryptophan to 5HTP to serotonin pathway noted by Dr. Juhl. In his 2003 book titled Treating and beating Fibromyalgia and Chronic Fatigue Syndrome, Dr. Murphree suggests supplementing with 100-300 mg of 5HTP on an empty stomach 30 minutes before bed. He notes that it can take several nights to two weeks before supplementing with 5HTP starts to work.
LOW LEVEL LASER THERAPY
Below are 3 studies that show significant benefit to management of chronic pain and fibromyalgia using low-level laser therapy. The first article is by Green, et al in 2000. The authors claim excellent positive therapeutic results in treating patients with chronic painful diabetic neuropathy, chronic myofascial pain, or complex regional pain syndrome.
Green et al conclude, "It appears that photon stimulation carries with it a significant potential for amelioration of chronic pain in which autonomic and neurovascular abnormalities are, in fact, present."
The second article is a randomized controlled clinical trial done in 2002 by Gur et al on patients with fibromyalgia. The laser group of patients were treated for 3 minutes at each tender point daily for 2 weeks. The authors note "Significant improvements were indicated in all clinical parameters in the laser group," and that "laser therapy can be used as a monotherapy or as a supplementary treatment to other therapeutic procedures in fibromyalgia."
Gur and others also publish the third article published in 2002. It is a single-blinded placebo-controlled trial of low power laser therapy in 40 female patients with fibromyalgia. The authors note that there was a "significant difference was in parameters as pain, muscle spasm, morning stiffness and tender point numbers in favour of laser group." These authors conclude "Our study suggests that laser therapy is effective on pain, muscle spasm, morning stiffness, and total tender point number in fibromyalgia and suggests that this therapy method is a safe and effective way of treatment in the cases with fibromyalgia."
According to Jan Tuner, and Lars Hode's 2002 text titled Laser Therapy, Clinical Practice and Scientific Background, the first low level laser to be awarded 510K market clearance by the United States Food and Drug Administration is from Erchonia Medical. Erchonia medical is located in McKinney, TX: (888) 242-0571.
According to a book chapter titled "Low-Power Laser Therapy" by Tina Karu, low-level laser therapy physiologically increases the mitochondrial production on cellular energy ATP. This is similar to the proposed mechanism of supplementing with malic acid and magnesium, as noted above.
EXCITOTOXINS
Below are listed 5 books that deal extensively with dietary excitotoxins and their deleterious effects on human physiology. These deleterious effects include chronic fibromyalgia pain because dietary excitotoxins also function as excitatory neurotransmitters for chronic pain (Dickenson).
In a nutshell, dietary excitotoxins are added to food because they function as excitatory neurotransmitters, enhancing the flavor of food. The two main dietary excitotoxins are glutamate (often labeled monosodium glutamate or MSG, and aspartame because it is metabolized to the excitotoxin aspartate).
In excess, these substances can literally excite neurons to death, and therefore have been associated with neurodegenerative diseases such as Alzheimer and Parkinson diseases, as well as a plethora of other symptoms, including fibromyalgia chronic pain. Unfortunately, excitotoxins such as glutamate can have dozens of names on food labels.
In 2001, Smith reports on 4 cases of chronic pain fibromyalgia patients who where successfully treated after avoiding all products that contain the excitotoxins glutamate and aspartame. Some of these patients had suffered for as long as 17 years, and were taking as many as 13 different drugs for their symptoms.
Smith notes the following:
"Excitotoxins are molecules, such as MSG and aspartate that act as excitatory neurotransmitters, and can lead to neurotoxicity when used in excess."
"MSG, the sodium salt of the amino acid glutamic acid or glutamate, is an additive used to enhance the flavor of certain foods."
The US Food and Drug Administration (FDA) grandfathered MSG, like salt and baking powder, as harmless food substances in 1959.
Aspartame was first marketed in 1981, and is a dipeptide of aspartate and phenylalanine used in foods, beverages, and drugs.
"In animal models, aspartame has been associated with an increased incidence of brain tumors."
"Anecdotally, aspartame use in humans has been linked with head aches, seizures, dizziness, movement disorders, urticaria, angioedema, and anaphylaxis."
"Much of the research performed proving that glutamate was safe for human consumption may have been flawed."
Glutamate has a role in chronic pain sensitization:
"MSG is nearly ubiquitous in processed food, appearing under many names, including gelatin, hydrolyzed vegetable protein, textured protein, and yeast extract."
Aspartame is the dominant artificial sweetener on the market since 1981.
Fibromyalgia can be caused by exposure to dietary excitotoxins in susceptible individuals.
Aspartate and glutamate taken together have additive neurotoxic effects.
The elimination of MSG and other excitotoxins from the diets of patients with fibromyalgia offers a benign treatment option that has the potential for dramatic results in a subset of patients.
There are dozens of names for glutamate as it is added to foods. A partial list of names seen on food packaging are listed below, from the website www.truthinlabeling.org:
HIDDEN SOURCES OF PROCESSED FREE GLUTAMIC ACID (MSG)
Autolyzed, hydrolyzed, glutamate, glutamic acid, hydrolyzed, autolyzed
NAMES OF INGREDIENTS THAT CONTAIN ENOUGH MSG TO SERVE AS COMMON MSG-REACTION TRIGGERS
The MSG-reaction is a reaction to free glutamic acid that occurs in food as a consequence of manufacture. MSG-sensitive people do not react to protein (which contains bound glutamic acid) or any of the minute amounts of free glutamic acid that might be found in unadulterated, unfermented, food.
These ALWAYS contain MSG
Glutamate
Glutamic acid
Gelatin
Monosodium glutamate
Calcium caseinate
Textured protein
Monopotassium glutamate
Sodium caseinate
Yeast nutrient
Yeast extract
Yeast food
Autolyzed yeast
Hydrolyzed protein (any protein that is hydrolyzed) Hydrolyzed corn gluten
These OFTEN contain MSG or create MSG during processing
Carrageenan
Maltodextrin
Malt extract
Natural pork flavoring
Citric acid Malt flavoring
Bouillon and Broth Natural chicken flavoring Soy protein isolate
Natural beef flavoring
Ultra-pasteurized Soy sauce
Stock Barley malt
Soy sauce extract
Whey protein concentrate Pectin
Soy protein
Whey protein Protease
Soy protein concentrate
Whey protein isolate
Protease enzymes
Anything protein fortified
Flavors(s) & Flavoring(s)
Anything fermented Anything enzyme modified
Enzymes anything
Seasonings Natural flavor & flavoring (the word "seasonings")
The website further notes that "The new game is to label hydrolyzed proteins as pea protein, whey protein, corn protein, etc. If a pea, for example, were whole, it would be identified as a pea. Calling an ingredient pea protein indicates that the pea has been hydrolyzed, at least in part, and that processed free glutamic acid (MSG) is present."
"MSG reactions have been reported to soaps, shampoos, hair conditioners, and cosmetics, where MSG is hidden in ingredients that include the words 'hydrolyzed,' 'amino acids,' and 'protein.' Low fat and no fat milk products often include milk solids that contain MSG. Drinks, candy, and chewing gum are potential sources of hidden MSG and of aspartame and neotame."
"Aspartic acid, found in neotame and aspartame (NutraSweet), ordinarily causes MSG type reactions in MSG sensitive people. Aspartame is found in some medications, including children's medications."
"According to the manufacturer, Varivax–Merck chicken pox vaccine (Varicella Virus Live), contains L-monosodium glutamate and hydrolyzed gelatin both of which contain processed free glutamic acid (MSG) which cause brain lesions in young laboratory animals, and cause endocrine disturbances like obesity and reproductive disorders later in life. It would appear that most, if not all, live virus vaccines contain MSG."
Fibromyalgia patients are often quite resistant to traditional treatment approaches. Today's chiropractors used all or some of the above adjuncts, along with traditional joint adjusting, tissue work, postural improvement and exercise. Most patients so treated experience substantial benefit and achieve acceptable clinical improvement.
REFERENCES
Abraham GE, Flechas JD. Management of Fibromyalgia: Rationale for the Use of Magnesium and Malic Acid. J of Nutritional Med. 1992 (3) 49-59.
A. W. Al-Allaf, K. L. Dunbar, N. S. Hallum, B. Nosratzadeh, K. D. Templeton and
T. Pullar. A case–control study examining the role of physical trauma in the onset of fibromyalgia syndrome Rheumatology 2002; 41: 450-453.
Borut Banic, Steen Petersen-Felix, Ole K. Andersen, Bogdan P. Radanov, P. M. Villiger, Lars Arendt-Nielse and Michele Curatolo. Evidence for spinal cord hypersensitivity in chronic pain after whiplash injury and in fibromyalgia. Pain. January 2004, Pages 7-15.
Buskila D, Neumann L, Vaisberg G, Alkalay D, Wolfe F. Increased rates of fibromyalgia following cervical spine injury. A controlled study of 161 cases of traumatic injury. Arthritis Rheum. 1997 Mar;40(3):446-52.
Dickenson AH. Gate Control Theory of pain stands the test of time British Journal of Anaesthesia, Vol. 88, No. 6, June 2002, Pgs. 755-757.
Green J, Fralicker D, Clewell W, Horowitz E, Lucey T, Yannacone V, Haber C. INFRARED PHOTON STIMULATION: A NEW FORM OF CHRONIC PAIN
THERAPY. American Journal of Pain Management, Vol. 10, No. 3 July 2000,113-120;
Greenfield S, Fitzcharles MA, Esdaile JM. Reactive fibromyalgia syndrome.
Arthritis Rheum. 1992 Jun;35(6):678-81.
Gur A, Karakoc M, Nas K, Cevik R, Sarac J, Ataoglu S. Effects of low power laser and low dose amitriptyline therapy on clinical symptoms and quality of life in fibromyalgia: a single-blind, placebo-controlled trial. Rheumatol Int. 2002 Sep;22(5):188-93.
Gur A, Karakoc M, Nas K, Cevik R, Sarac J, Demir E. Efficacy of low power laser therapy in fibromyalgia: a single-blind, placebo-controlled trial. Lasers Med Sci. 2002;17(1):57-61.
Juhl JH, (1998-10-01). "Fibromyalgia and the serotonin pathway",
Altern Med Rev;3(5):367-75.
Karu, Tina, "Low-Power Laser Therapy", Chapter 48 in Biomedical Photonics Handbook, Tuan Vo-Dinh, CRS Press, 2003.
Murphree, Rodger, Treating and beating Fibromyalgia and Chronic Fatigue Syndrome, The Definitive Guide for Patients and Physicians, Harrison and Hampton Publishing, 2003.
Neumann L, Zeldets V, Bolotin A, Buskila D. Outcome of posttraumatic fibromyalgia: A 3-year follow-up of 78 cases of cervical spine injuries.
Semin Arthritis Rheum. 2003 Apr;32(5):320-5.
Russell IJ, Michalek JE, Flechas JD, Abraham GE. Treatment of fibromyalgia syndrome with Super Malic: a randomized, double blind, placebo controlled, crossover pilot study. J Rheumatol. 1995 May;22(5):953-8.
Smith JD, Terpening CM, Schmidt SOF, Gums JG. Relief of Fibromyalgia Symptoms Following Discontinuation of Dietary Excitotoxins The Annals of Pharmacotherapy: Vol. 35, No. 6, pp. 702–706. June 2001
Tuner, Jan and Hode, Lars, Laser Therapy, Clinical Practice and Scientific Background, Prima Books, 2002.
Waylonis GW, Perkins RH. Post-traumatic fibromyalgia. A long-term follow-up.
Am J Phys Med Rehabil. 1994 Nov-Dec;73(6):403-12.
Excitotoxin Books
Excitotoxins, The Taste That Kills by Russell Blaylock (University of Mississippi neurosurgeon), Health Press, 1997
In Bad Taste, The MSG Symptom Complex, by George Schwartz, Health Press, 1999
The Crazy Makers, How the Food Industry Is Destroying Our Brains and Harming Our Children, by Carol Simontacchi, Tarcher Putnam, 2000
Food Allergies by William Walsh, Wiley, 2000
Health and Nutrition Secrets by Russell Blaylock, Heath press, 2006
Fibromyalgia Article Summary
A case–control study examining the role of physical
trauma in the onset of fibromyalgia syndrome
Rheumatology 2002; 41: 450-453
A. W. Al-Allaf, K. L. Dunbar, N. S. Hallum, B. Nosratzadeh, K. D. Templeton and
T. Pullar
FROM ABSTRACT
Objective.
To investigate whether physical trauma may precipitate the onset of fibromyalgia syndrome (FMS).
Design.
A case–control study was carried out to compare fibromyalgia out-patients with controls attending non-rheumatology out-patient clinics.
Method.
136 FMS patients and 152 age- and sex-matched controls completed a postal questionnaire about any physical trauma in the 6 months before the onset of their symptoms.
Results.
Fifty-three (39%) FMS patients reported significant physical trauma in the 6 months before the onset of their disease, compared with only 36 (24%) of controls (P<0.007).
There was no significant difference between FMS patients who had a history of physical trauma and those who did not have physical trauma with regard to age, sex, disease duration, employment status and whether their job at onset was manual.
Conclusion.
Physical trauma in the preceding 6 months is significantly associated with the onset of FMS.
KEY POINTS
(1) Fibromyalgia is the 3rd or 4th most common rheumatological referral.
(2) 2% of the population has fibromyalgia, primarily in women.
(3) Physical trauma is a significantly etiological trigger for FMS onset.
(4) 25% to 50% of those with FMS note physical trauma immediately prior the onset.
(5) The risk of developing FMS is more than 10-fold higher in adults with neck injuries than in other adults (1997 study).
(6) Those who develop FMS after trauma may be "genetically predisposed."
(7) Physical trauma is also increases the risk for osteoarthritis, rheumatoid arthritis, psoriasis and ankylosing spondylitis.
Treatment of fibromyalgia syndrome with Super Malic:
a randomized, double blind, placebo controlled, crossover pilot study
Journal of Rheumatology, May 1995;22(5):953-8
Russell IJ, Michalek JE, Flechas JD, Abraham GE.
FROM ABSTRACT
OBJECTIVE.
To study the efficacy and safety of Super Malic, a proprietary tablet containing malic acid (200 mg) and magnesium (50 mg), in treatment of primary fibromyalgia syndrome.
The 3 primary outcome variables were measures of pain and tenderness but functional and psychological measures were also assessed.
RESULTS.
With dose escalation and a longer duration of treatment in the open label trial, significant reductions in the severity of all 3 primary pain/tenderness measures were obtained without limiting risks.
CONCLUSIONS.
These data suggest that Super Malic is safe and may be beneficial in the treatment of patients with fibromyalgia.
KEY POINTS FROM THIS ARTICLE
1) An explanation for the soft tissue pain experienced by patients with fibromyalgia was that muscle energy production of ATP may be compromised.
2) Also, abnormal blood flow may deprive muscle of sufficient oxygen and other nutrients.
3) The muscles of patients with fibromyalgia are deficient in ATP and magnesium.
4) Malic acid and magnesium "play a pivotal role in mitochondrial ATP synthesis."
5) Malic acid is "widely distributed in the vegetable kingdom including concentrations of 4 to 8 g/l of apple juice."
6) Malic acid plus magnesium can increase mitochondrial production of ATP energy.
7) The best results were observed from "use of a higher dosage and longer duration of treatment" with malic acid and magnesium.
8) Study results "indicate that it may be beneficial on the painful fibromyalgia symptoms in dosages in excess of 8 tablets/day for up to 6 months."
[8 tablets X 200 mg per tablet = 1600 mg malic acid per day]
[8 tablets X 50 mg per tablet = 400 mg magnesium per day]
9) The proposed mechanism for the benefit of malic acid plus magnesium supplementation is that they "increase production of ATP."
Evidence for spinal cord hypersensitivity in chronic pain after whiplash injury and in fibromyalgia
Pain, January 2004, Pages 7-15
Borut Banic, Steen Petersen-Felix, Ole K. Andersen, Bogdan P. Radanov, P. M. Villiger, Lars Arendt-Nielse and Michele Curatolo
FROM ABSTRACT:
Patients with chronic pain after whiplash injury and fibromyalgia patients display exaggerated pain after sensory stimulation.
Because evident tissue damage is usually lacking, this exaggerated pain perception could be explained by hyperexcitability of the central nervous system.
The nociceptive withdrawal reflex (a spinal reflex) may be used to study the excitability state of spinal cord neurons.
We tested the hypothesis that patients with chronic whiplash pain and fibromyalgia display facilitated withdrawal reflex and therefore spinal cord hypersensitivity.
Three groups were studied: whiplash (n=27), fibromyalgia (n=22) and healthy controls (n=29).
Two types of transcutaneous electrical stimulation of the sural nerve were applied: single stimulus and five repeated stimuli at 2 Hz. Electromyography was recorded from the biceps femoris muscle. The main outcome measurement was the minimum current intensity eliciting a spinal reflex (reflex threshold).
Reflex thresholds were significantly lower in the whiplash compared with the control group, after both single and repeated stimulation.
The same was observed for the fibromyalgia group, after both stimulation modalities.
We provide evidence for spinal cord hyperexcitability in patients with chronic pain after whiplash injury and in fibromyalgia patients.
This can cause exaggerated pain following low intensity nociceptive or innocuous peripheral stimulation.
Spinal hypersensitivity may explain, at least in part, pain in the absence of detectable tissue damage.
KEY POINTS FROM THIS ARTICLE
1) Whiplash causes tissue damage.
2) This tissue damage is not recognized by available diagnostic procedures.
3) Whiplash tissue damage produces inflammation.
4) This inflammation alters the thresholds of the nociceptive afferent system, increasing pain.
5) This inflammation also induces a gene expression in the dorsal root ganglion resulting in increased peripheral receptor fields. [Receptive Field Enlargement]
This also increases pain.
6) This inflammation also increases the expression (production) of cyclooxygenase-2 (COX-2) in the spinal cord, which is an enzyme that converts the omega-6 fatty acid arachidonic acid into the pro-inflammatory eicosanoid prostaglandin E2. The pro-inflammatory eicosanoid prostaglandin E2 further alters the thresholds of the nociceptive afferent system, sending more pain afferentation into the spinal cord.
7) This increased COX-2 expression is not confined to the neural structures connected to the site of inflammation, but is observed in the whole spinal cord and in supraspinal centers. This alters the pain sensitivity of the entire body, including non-injured regions.
8) All of this induces profound plasticity changes [synaptogenesis/neuroplasticity] in the spinal cord that result in increased pain that can persist after all possible tissue healing has occurred.
9) Some of these spinal plastic changes may be irreversible (permanent chronic pain syndromes).
10) This article objectively proves that patients with chronic pain have hypersensitivity of the spinal cord neurons.
11) The absence of evident tissue damage does not necessarily mean that there is no tissue damage.
12) Elevated levels of excitatory amino acids, like glutamate, are often found in the cerebrospinal fluid of chronic pain patients, and cause generalized spinal cord hyperexcitability.
14) Serotonin inhibits pain and inhibits depression. Reduced serotonin may explain while chronic pain patients often suffer from psychological distress.
Relief of Fibromyalgia Symptoms Following Discontinuation of Dietary Excitotoxins
The Annals of Pharmacotherapy: Vol. 35, No. 6, pp. 702–706.
June 2001
Jerry D Smith, Chris M Terpening, Siegfried OF Schmidt and John G Gums
FROM ABSTRACT:
BACKGROUND:
Fibromyalgia is a common rheumatologic disorder that is often difficult to treat effectively.
CASE SUMMARY:
Four patients diagnosed with fibromyalgia syndrome for two to 17 years are described. All had undergone multiple treatment modalities with limited success.
All had complete, or nearly complete, resolution of their symptoms within months after eliminating monosodium glutamate (MSG) or MSG plus aspartame from their diet.
All patients were women with multiple comorbidities prior to elimination of MSG.
All have had recurrence of symptoms whenever MSG is ingested.
DISCUSSION:
Excitotoxins are molecules, such as MSG and aspartate that act as excitatory neurotransmitters, and can lead to neurotoxicity when used in excess.
We propose that these four patients may represent a subset of fibromyalgia syndrome that is induced or exacerbated by excitotoxins or, alternatively, may comprise an excitotoxin syndrome that is similar to fibromyalgia.
CONCLUSIONS:
The elimination of MSG and other excitotoxins from the diets of patients with fibromyalgia offers a benign treatment option that has the potential for dramatic results in a subset of patients.
KEY POINTS FROM THIS ARTICLE:
1) Fibromyalgia is common difficult to treat.
2) Fibromyalgia can be caused by exposure to dietary excitotoxins in susceptible individuals.
3) Excitotoxins are molecules, such as MSG and aspartate, that act as excitatory neurotransmitters.
4) MSG is found in nearly all processed food and can have many names, including gelatin, hydrolyzed vegetable protein, textured protein, and yeast extract."
5) Aspartame is the dominant artificial sweetener on the market since 1981.
6) Glutamate and other dietary excitotoxins primarily enter the brain at the hypothalamus that is not well protected by the blood-brain barrier.
7) Glutamate is the neurotransmitter that causes dorsal horn spinal cord chronic pain sensitization.
8) Aspartate and glutamate taken together have additive neurotoxic effects.
9) Much of the research done to show that glutamate was safe for human consumption may have been flawed.
10) The elimination of MSG and other excitotoxins from the diets of patients with fibromyalgia offers a benign treatment option that has the potential for dramatic results in a subset of patients.


